Targeting the sarcomere to correct muscle function
Various human diseases can disrupt the balance between muscle contraction and relaxation. Sarcomeric modulators can be used to readjust this balance either indirectly by intervening in signalling pathways or directly through interaction with the muscle proteins that control contraction. Such agents represent a novel approach to treating any condition in which striated muscle function is compromised, including heart failure, cardiomyopathies, skeletal myopathies and a wide range of neuromuscular conditions. Here, we review agents that modulate the mechanical function of the sarcomere, focusing on emerging compounds that target myosin or the troponin complex.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
206,07 € per year
only 17,17 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others

Aficamten is a small-molecule cardiac myosin inhibitor designed to treat hypertrophic cardiomyopathy
Article Open access 23 July 2024

Targeting the sarcomere in inherited cardiomyopathies
Article 18 March 2022

Modulation of myosin by cardiac myosin binding protein-C peptides improves cardiac contractility in ex-vivo experimental heart failure models
Article Open access 14 March 2022
References
- Huxley, H. & Hanson, J. Changes in the cross-striations of muscle during contraction and stretch and their structural interpretation. Nature173, 973–976 (1954). ArticleCASPubMedGoogle Scholar
- Knoll, R. & Marston, S. On mechanosensation, acto/myosin interaction, and hypertrophy. Trends Cardiovasc. Med.22, 17–22 (2012). ArticleCASPubMedGoogle Scholar
- Kolb, S. J. & Kissel, J. T. Spinal muscular atrophy: a timely review. Arch. Neurol.68, 979–984 (2011). ArticlePubMedGoogle Scholar
- Rowland, L. P. & Shneider, N. A. Amyotrophic lateral sclerosis. N. Engl. J. Med.344, 1688–1700 (2001). ArticleCASPubMedGoogle Scholar
- Shefner, J. M., Wolff, A. A. & Meng, L. The relationship between tirasemtiv serum concentration and functional outcomes in patients with ALS. Amyotroph. Lateral Scler. Frontotemporal Degener.14, 582–585 (2013). ArticleCASPubMedGoogle Scholar
- Chou, R., Peterson, K. & Helfand, M. Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review. J. Pain Symptom Manage.28, 140–175 (2004). ArticleCASPubMedGoogle Scholar
- Desai, A. S. & Stevenson, L. W. Rehospitalization for heart failure: predict or prevent? Circulation126, 501–506 (2012). ArticlePubMedGoogle Scholar
- Curtis, J. P. et al. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J. Am. Coll. Cardiol.42, 736–742 (2003). ArticlePubMedGoogle Scholar
- Lam, C. S., Donal, E., Kraigher-Krainer, E. & Vasan, R. S. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur. J. Heart Fail.13, 18–28 (2011). ArticlePubMedGoogle Scholar
- Lovelock, J. D. et al. Ranolazine improves cardiac diastolic dysfunction through modulation of myofilament calcium sensitivity. Circ. Res.110, 841–850 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Boswell-Smith, V., Spina, D. & Page, C. P. Phosphodiesterase inhibitors. Br. J. Pharmacol.14, S252–S257 (2006). ArticleCASGoogle Scholar
- Bers, D. M. Calcium fluxes involved in control of cardiac myocyte contraction. Circ. Res.87, 275–281 (2000). ArticleCASPubMedGoogle Scholar
- Marks, A. R. Calcium cycling proteins and heart failure: mechanisms and therapeutics. J. Clin. Invest.123, 46–52 (2013). ArticleCASPubMedPubMed CentralGoogle Scholar
- Gailly, P. New aspects of calcium signaling in skeletal muscle cells: implications in Duchenne muscular dystrophy. Biochim. Biophys. Acta1600, 38–44 (2002). ArticleCASPubMedGoogle Scholar
- Stanley, W. C., Recchia, F. A. & Lopaschuk, G. D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev.85, 1093–1129 (2005). ArticleCASPubMedGoogle Scholar
- Egan, B. & Zierath, J. R. Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell. Metab.17, 162–184 (2013). ArticleCASPubMedGoogle Scholar
- McCarthy, J. J. & Esser, K. A. Anabolic and catabolic pathways regulating skeletal muscle mass. Curr. Opin. Clin. Nutr. Metab. Care13, 230–235 (2010). ArticleCASPubMedPubMed CentralGoogle Scholar
- Frey, N. & Olson, E. N. Cardiac hypertrophy: the good, the bad, and the ugly. Annu. Rev. Physiol.65, 45–79 (2003). ArticleCASPubMedGoogle Scholar
- Barry, S. P., Davidson, S. M. & Townsend, P. A. Molecular regulation of cardiac hypertrophy. Int. J. Biochem. Cell Biol.40, 2023–2039 (2008). ArticleCASPubMedGoogle Scholar
- Endoh, M. Amrinone, forerunner of novel cardiotonic agents, caused paradigm shift of heart failure pharmacotherapy. Circ. Res.113, 358–361 (2013). ArticleCASPubMedGoogle Scholar
- Sato, S., Talukder, M. A., Sugawara, H., Sawada, H. & Endoh, M. Effects of levosimendan on myocardial contractility and Ca 2+ transients in aequorin-loaded right-ventricular papillary muscles and indo-1-loaded single ventricular cardiomyocytes of the rabbit. J. Mol. Cell Cardiol30, 1115–1128 (1998). ArticleCASPubMedGoogle Scholar
- Kawabata, Y. & Endoh, M. Effects of the positive inotropic agent Org 30029 on developed force and aequorin light transients in intact canine ventricular myocardium. Circ. Res.72, 597–606 (1993). ArticleCASPubMedGoogle Scholar
- Miller, D. J. & Steele, D. S. The 'calcium sensitising' effects of ORG30029 in saponin- or Triton-skinned rat cardiac muscle. Br. J. Pharmacol.100, 843–849 (1990). ArticleCASPubMedPubMed CentralGoogle Scholar
- Solaro, R. J., Pang, D. C. & Briggs, F. N. The purification of cardiac myofibrils with Triton X-100. Biochim. Biophys. Acta245, 259–262 (1971). ArticleCASPubMedGoogle Scholar
- Fiske, C. H. & Subbarow, Y. The colorimetric determination of phosphorus. J. Biol. Chem.66, 375–400 (1925). ArticleCASGoogle Scholar
- Papp, Z. et al. Levosimendan: molecular mechanisms and clinical implications: consensus of experts on the mechanisms of action of levosimendan. Int. J. Cardiol.159, 82–87 (2012). ArticlePubMedGoogle Scholar
- Boyle, K. L. & Leech, E. A review of the pharmacology and clinical uses of pimobendan. J. Vet. Emerg. Crit. Care (San Antonio)22, 398–408 (2012). ArticleGoogle Scholar
- van Meel, J. C., Zimmermann, R., Diederen, W., Erdman, E. & Mrwa, U. Increase in calcium sensitivity of cardiac myofibrils contributes to the cardiotonic action of sulmazole. Biochem. Pharmacol.37, 213–220 (1988). ArticleCASPubMedGoogle Scholar
- Bethke, T. et al. High selectivity for inhibition of phosphodiesterase III and positive inotropic effects of MCI-154 in guinea pig myocardium. J. Cardiovasc. Pharmacol.21, 847–855 (1993). ArticleCASPubMedGoogle Scholar
- Sugawara, H. et al. Investigation on SCH00013, a novel cardiotonic agent with Ca ++ sensitizing action. 3rd communication: stereoselectivity of the enantiomers in cardiovascular effects. Arzneimittelforschung49, 412–419 (1999). CASPubMedGoogle Scholar
- de Boer, J. et al. Human bronchial cyclic nucleotide phosphodiesterase isoenzymes: biochemical and pharmacological analysis using selective inhibitors. Br. J. Pharmacol.106, 1028–1034 (1992). ArticleCASPubMedPubMed CentralGoogle Scholar
- Keravis, T. & Lugnier, C. Cyclic nucleotide phosphodiesterase (PDE) isozymes as targets of the intracellular signalling network: benefits of PDE inhibitors in various diseases and perspectives for future therapeutic developments. Br. J. Pharmacol.165, 1288–1305 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Bethke, T. et al. Phosphodiesterase inhibition by enoximone in preparations from nonfailing and failing human hearts. Arzneimittelforschung42, 437–445 (1992). CASPubMedGoogle Scholar
- Szilagyi, S. et al. The effects of levosimendan and OR-1896 on isolated hearts, myocyte-sized preparations and phosphodiesterase enzymes of the guinea pig. Eur. J. Pharmacol.486, 67–74 (2004). A detailed study of the effective concentrations of levosimendan and its active metabolite, OR-1896, with respect to positive inotropic activity, calcium sensitization and inhibition of PDE3 and PDE4.ArticleCASPubMedGoogle Scholar
- Mika, D. et al. Differential regulation of cardiac excitation–contraction coupling by cAMP phosphodiesterase subtypes. Cardiovasc. Res.100, 336–346 (2013). ArticleCASPubMedPubMed CentralGoogle Scholar
- Roubille, F. & Tardif, J. C. New therapeutic targets in cardiology: heart failure and arrhythmia: HCN channels. Circulation127, 1986–1996 (2013). ArticlePubMedGoogle Scholar
- Perera, R. K. & Nikolaev, V. O. Compartmentation of cAMP signalling in cardiomyocytes in health and disease. Acta Physiol. (Oxf.)207, 650–662 (2013). ArticleCASGoogle Scholar
- Cazorla, O., Lucas, A., Poirier, F., Lacampagne, A. & Lezoualc'h, F. The cAMP binding protein Epac regulates cardiac myofilament function. Proc. Natl Acad. Sci. USA106, 14144–14149 (2009). A unique study showing that cardiac calcium sensitivity can be enhanced through a novel pathway involving EPAC, PKC, calcium/calmodulin kinase II, and an uncharacterized phosphorylation site on cardiac troponin I.ArticleCASPubMedPubMed CentralGoogle Scholar
- Wendt, I. R. & Stephenson, D. G. Effects of caffeine on Ca-activated force production in skinned cardiac and skeletal muscle fibres of the rat. Pflugers Arch.398, 210–216 (1983). ArticleCASPubMedGoogle Scholar
- Parsons, W. J., Ramkumar, V. & Stiles, G. L. The new cardiotonic agent sulmazole is an A1 adenosine receptor antagonist and functionally blocks the inhibitory regulator, Gi. Mol. Pharmacol.33, 441–448 (1988). This study uniquely describes the cross-reactivity between PDE3 inhibition and adenosine receptor antagonism of several compounds.CASPubMedGoogle Scholar
- Kitada, Y., Kobayashi, M., Narimatsu, A. & Ohizumi, Y. Potent stimulation of myofilament force and adenosine triphosphatase activity of canine cardiac muscle through a direct enhancement of troponin C Ca ++ binding by MCI-154, a novel cardiotonic agent. J. Pharmacol. Exp. Ther.250, 272–277 (1989). CASPubMedGoogle Scholar
- Haikala, H. et al. Cardiac troponin C as a target protein for a novel calcium sensitizing drug, levosimendan. J. Mol. Cell Cardiol.27, 1859–1866 (1995). ArticleCASPubMedGoogle Scholar
- Pollesello, P. et al. Binding of a new Ca 2+ sensitizer, levosimendan, to recombinant human cardiac troponin C. A molecular modelling, fluorescence probe, and proton nuclear magnetic resonance study. J. Biol. Chem.269, 28584–28590 (1994). ArticleCASPubMedGoogle Scholar
- Kleerekoper, Q. & Putkey, J. A. Drug binding to cardiac troponin C. J. Biol. Chem.274, 23932–23939 (1999). ArticleCASPubMedGoogle Scholar
- Sorsa, T., Pollesello, P., Permi, P., Drakenberg, T. & Kilpelainen, I. Interaction of levosimendan with cardiac troponin C in the presence of cardiac troponin I peptides. J. Mol. Cell Cardiol.35, 1055–1061 (2003). ArticleCASPubMedGoogle Scholar
- Robertson, I. M., Baryshnikova, O. K., Li, M. X. & Sykes, B. D. Defining the binding site of levosimendan and its analogues in a regulatory cardiac troponin C-troponin I complex. Biochemistry47, 7485–7495 (2008). ArticleCASPubMedGoogle Scholar
- Sorsa, T. et al. Binding of levosimendan, a calcium sensitizer, to cardiac troponin C. J. Biol. Chem.276, 9337–9343 (2001). ArticleCASPubMedGoogle Scholar
- Orstavik, O. et al. PDE3-inhibition by levosimendan is sufficient to account for its inotropic effect in failing human heart. Br. J. Pharmacol.171, 5169–5181 (2014). ArticleCASPubMedPubMed CentralGoogle Scholar
- Bodi, A., Szilagyi, S., Edes, I. & Papp, Z. The cardiotonic effects of levosimendan in guinea pig hearts are modulated by β-adrenergic stimulation. Gen. Physiol. Biophys.22, 313–327 (2003). CASPubMedGoogle Scholar
- Erdei, N., Papp, Z., Pollesello, P., Edes, I. & Bagi, Z. The levosimendan metabolite OR-1896 elicits vasodilation by activating the KATP and BKCa channels in rat isolated arterioles. Br. J. Pharmacol.148, 696–702 (2006). ArticleCASPubMedPubMed CentralGoogle Scholar
- Yoshida, H. et al. A phosphodiesterase 3 inhibitor, K-134, improves hindlimb skeletal muscle circulation in rat models of peripheral arterial disease. Atherosclerosis221, 84–90 (2012). ArticleCASPubMedGoogle Scholar
- Nieminen, M. S. et al. Levosimendan: current data, clinical use and future development. Heart Lung Vessel5, 227–245 (2013). CASPubMedPubMed CentralGoogle Scholar
- Landoni, G. et al. Effects of levosimendan on mortality and hospitalization. A meta-analysis of randomized controlled studies. Crit. Care Med.40, 634–646 (2012). ArticleCASPubMedGoogle Scholar
- Mebazaa, A. et al. Levosimendan versus dobutamine for patients with acute decompensated heart failure: the SURVIVE randomized trial. JAMA297, 1883–1891 (2007). A report of one of the largest multi-centre trials involving the calcium sensitizer levosimendan, showing no mortality benefit, which is in contrast to several smaller trials.ArticleCASPubMedGoogle Scholar
- Packer, M. et al. Effect of levosimendan on the short-term clinical course of patients with acutely decompensated heart failure. JACC Heart Fail.1, 103–111 (2013). This study reports the REVIVE II trial results on levosimedan, which had a similar outcome to the SURVIVE trial. Publication of the REVIVE II results was delayed for many years.ArticlePubMedGoogle Scholar
- Packer, M. et al. Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group. N. Engl. J. Med.325, 1468–1475 (1991). ArticleCASPubMedGoogle Scholar
- Amsallem, E., Kasparian, C., Haddour, G., Boissel, J. P. & Nony, P. Phosphodiesterase III inhibitors for heart failure. Cochrane Database Syst. Rev.1, CD002230 (2005). Google Scholar
- Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol62, e147–e239 (2013). ArticlePubMedGoogle Scholar
- McMurray, J. J. et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J.33, 1787–1847 (2012). ArticlePubMedGoogle Scholar
- Baudenbacher, F. et al. Myofilament Ca 2+ sensitization causes susceptibility to cardiac arrhythmia in mice. J. Clin. Invest.118, 3893–3903 (2008). CASPubMedPubMed CentralGoogle Scholar
- Parry, D. A. & Squire, J. M. Structural role of tropomyosin in muscle regulation: analysis of the X-ray diffraction patterns from relaxed and contracting muscles. J. Mol. Biol.75, 33–55 (1973). ArticleCASPubMedGoogle Scholar
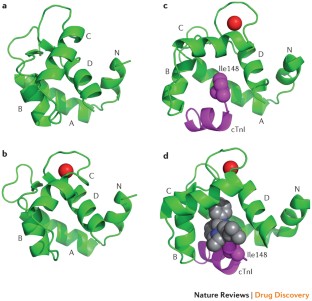
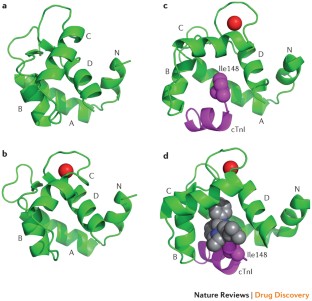
- Li, M. X., Spyracopoulos, L. & Sykes, B. D. Binding of cardiac troponin-I147-163 induces a structural opening in human cardiac troponin-C. Biochemistry38, 8289–8298 (1999). ArticleCASPubMedGoogle Scholar
- Rieck, D. C., Li, K. L., Ouyang, Y., Solaro, R. J. & Dong, W. J. Structural basis for the in situ Ca 2+ sensitization of cardiac troponin C by positive feedback from force-generating myosin cross-bridges. Arch. Biochem. Biophys.537, 198–209 (2013). ArticleCASPubMedGoogle Scholar
- Sweeney, H. L. & Houdusse, A. Structural and functional insights into the myosin motor mechanism. Annu. Rev. Biophys.39, 539–557 (2010). ArticleCASPubMedGoogle Scholar
- Webb, M. et al. The myosin duty ratio tunes the calcium sensitivity and cooperative activation of the thin filament. Biochemistry52, 6437–6444 (2013). ArticleCASPubMedGoogle Scholar
- Margossian, S. S. & Lowey, S. Preparation of myosin and its subfragments from rabbit skeletal muscle. Methods Enzymol.85, 55–71 (1982). ArticleCASPubMedGoogle Scholar
- Pardee, J. D. & Spudich, J. A. Purification of muscle actin. Methods Enzymol.85, 164–181 (1982). ArticleCASPubMedGoogle Scholar
- Smillie, L. B. Preparation and identification of α- and β-tropomyosins. Methods Enzymol.85, 234–241 (1982). ArticleCASPubMedGoogle Scholar
- Potter, J. D. Preparation of troponin and its subunits. Methods Enzymol.85, 241–263 (1982). ArticleCASPubMedGoogle Scholar
- Spudich, J. A. & Watt, S. The regulation of rabbit skeletal muscle contraction. I. Biochemical studies of the interaction of the tropomyosin–troponin complex with actin and the proteolytic fragments of myosin. J. Biol. Chem.246, 4866–4871 (1971). A classical paper describing the purification and reconstitution of myosin fragments, actin, troponin and tropomyosin.ArticleCASPubMedGoogle Scholar
- Malik, F. I. & Morgan, B. P. Cardiac myosin activation part 1: from concept to clinic. J. Mol. Cell Cardiol51, 454–461 (2011). A detailed description of the compound screening and development strategy that produced the cardiac myosin activator omecamtiv mecarbil.ArticleCASPubMedGoogle Scholar
- Malik, F. I. et al. Cardiac myosin activation: a potential therapeutic approach for systolic heart failure. Science331, 1439–1443 (2011). A comprehensive study of the binding of omecamtiv mecarbil to myosin, its effects on the actin–myosin crossbridging cycle, and its physiological effects on the heart.ArticleCASPubMedPubMed CentralGoogle Scholar
- Wang, Y., Ajtai, K. & Burghardt, T. P. Analytical comparison of natural and pharmaceutical ventricular myosin activators. Biochemistry53, 5298–5306 (2014). ArticleCASPubMedGoogle Scholar
- Wolska, B. M. et al. CGP-48506 increases contractility of ventricular myocytes and myofilaments by effects on actin–myosin reaction. Am. J. Physiol.270, H24–H32 (1996). CASPubMedGoogle Scholar
- Palmer, S., Di Bello, S., Davenport, S. L. & Herzig, J. W. The novel inotropic agent CGP 48506 alters force primarily by Ca 2+ -independent mechanisms in porcine skinned trabeculae. Cardiovasc. Res.32, 411–421 (1996). ArticleCASPubMedGoogle Scholar
- Brixius, K., Mehlhorn, U., Bloch, W. & Schwinger, R. H. Different effect of the Ca 2+ sensitizers EMD 57033 and CGP 48506 on cross-bridge cycling in human myocardium. J. Pharmacol. Exp. Ther.295, 1284–1290 (2000). A study of the contrasting effects of two myosin activators, EMD 57033 and CGP 48506, and one myosin inhibitor, butanedione monoxime, on calcium sensitivity, actin–myosin crossbridge cycling, force generation and tension cost.CASPubMedGoogle Scholar
- Ferroni, C. et al. A novel positive inotropic substance enhances contractility without increasing the Ca 2+ transient in rat myocardium. J. Mol. Cell Cardiol.23, 325–331 (1991). ArticleCASPubMedGoogle Scholar
- Solaro, R. J. et al. Stereoselective actions of thiadiazinones on canine cardiac myocytes and myofilaments. Circ. Res.73, 981–990 (1993). These authors show that EMD 57033 acts directly on the actin–myosin crossbridging cycle, making it one of the earliest identified myosin activators. Its enantiomer, EMD 57439, does not share this activity and is a more potent PDE inhibitor.ArticleCASPubMedGoogle Scholar
- Radke, M. B. et al. Small molecule-mediated refolding and activation of myosin motor function. Elife3, e01603 (2014). ArticlePubMedPubMed CentralCASGoogle Scholar
- Bond, L. M., Tumbarello, D. A., Kendrick-Jones, J. & Buss, F. Small-molecule inhibitors of myosin proteins. Future Med. Chem.5, 41–52 (2013). ArticleCASPubMedGoogle Scholar
- Allingham, J. S., Smith, R. & Rayment, I. The structural basis of blebbistatin inhibition and specificity for myosin II. Nature Struct. Mol. Biol.12, 378–379 (2005). This paper reports the atomic resolution structure of a sarcomeric myosin modulator, blebbistatin, bound to myosin. Other myosin modulators are believed to bind to different sites.ArticleCASGoogle Scholar
- Kovacs, M., Toth, J., Hetenyi, C., Malnasi-Csizmadia, A. & Sellers, J. R. Mechanism of blebbistatin inhibition of myosin II. J. Biol. Chem.279, 35557–35563 (2004). ArticleCASPubMedGoogle Scholar
- Rodriguez, H. M. et al. Modulation of the cardiac sarcomere by a small molecule agent MYK0000461: a potential therapeutic for the treatment of genetic hypertrophic cardiomyopathies. Biophys. J.106, 562a (2015). ArticleGoogle Scholar
- Teerlink, J. R. et al. Dose-dependent augmentation of cardiac systolic function with the selective cardiac myosin activator, omecamtiv mecarbil: a first-in-man study. Lancet378, 667–675 (2011). ArticleCASPubMedGoogle Scholar
- Cleland, J. G. et al. The effects of the cardiac myosin activator, omecamtiv mecarbil, on cardiac function in systolic heart failure: a double-blind, placebo-controlled, crossover, dose-ranging phase 2 trial. Lancet378, 676–683 (2011). ArticleCASPubMedGoogle Scholar
- Teerlink, J. R. & McDonagh, T. ATOMIC-AHF: acute treatment with omecamtiv mecarbil to increase contractility in acute heart failure: results from ATOMIC-AHF. European Society of Cardiology[online], (2013).
- Li, M. X. et al. Kinetic studies of calcium and cardiac troponin I peptide binding to human cardiac troponin C using NMR spectroscopy. Eur. Biophys. J.31, 245–256 (2002). ArticleCASPubMedGoogle Scholar
- Takeda, S., Yamashita, A., Maeda, K. & Maeda, Y. Structure of the core domain of human cardiac troponin in the Ca 2+ -saturated form. Nature424, 35–41 (2003). This important X-ray crystal structure remains the most comprehensive model of the cardiac troponin complex to date.ArticleCASPubMedGoogle Scholar
- Davis, J. P. et al. Effects of thin and thick filament proteins on calcium binding and exchange with cardiac troponin C. Biophys. J.92, 3195–3206 (2007). A fluorescently labelled cardiac troponin C effectively probes calcium affinity of the troponin complex in the presence of tropomyosin, actin and myosin, demonstrating how calcium sensitivity can be affected by all of these components.ArticleCASPubMedPubMed CentralGoogle Scholar
- Pineda-Sanabria, S. E., Julien, O. & Sykes, B. D. Versatile cardiac troponin chimera for muscle protein structural biology and drug discovery. ACS Chem. Biol.9, 2121–2130 (2014). ArticleCASPubMedGoogle Scholar
- Itoh, H., Tanaka, T., Mitani, Y. & Hidaka, H. The binding of the calcium channel blocker, bepridil, to calmodulin. Biochem. Pharmacol.35, 217–220 (1986). ArticleCASPubMedGoogle Scholar
- Solaro, R. J., Bousquet, P. & Johnson, J. D. Stimulation of cardiac myofilament force, ATPase activity and troponin C Ca ++ binding by bepridil. J. Pharmacol. Exp. Ther.238, 502–507 (1986). CASPubMedGoogle Scholar
- Li, Y., Love, M. L., Putkey, J. A. & Cohen, C. Bepridil opens the regulatory N-terminal lobe of cardiac troponin C. Proc. Natl Acad. Sci. USA97, 5140–5145 (2000). An X-ray crystal structure demonstrating how the calcium sensitizer bepridil stabilizes the calcium-bound open conformation of the regulatory N-terminal domain of troponin C.ArticleCASPubMedPubMed CentralGoogle Scholar
- Wang, X., Li, M. X. & Sykes, B. D. Structure of the regulatory N-domain of human cardiac troponin C in complex with human cardiac troponin I147-163 and bepridil. J. Biol. Chem.277, 31124–31133 (2002). NMR structures demonstrating how the calcium sensitizer bepridil binds in the interface between troponin C and the switch region of troponin I.ArticleCASPubMedGoogle Scholar
- Vinogradova, M. V. et al. Ca 2+ -regulated structural changes in troponin. Proc. Natl Acad. Sci. USA102, 5038–5043 (2005). This crystal structure of the fast skeletal muscle troponin complex serendipitously shows how anapoe detergent (used to enhance crystallization) binds to the interface between troponin C and troponin I to act as a calcium sensitizer.ArticleCASPubMedPubMed CentralGoogle Scholar
- Silver, P. J., Pinto, P. B. & Dachiw, J. Modulation of vascular and cardiac contractile protein regulatory mechanisms by calmodulin inhibitors and related compounds. Biochem. Pharmacol.35, 2545–2551 (1986). ArticleCASPubMedGoogle Scholar
- Adhikari, B. B. & Wang, K. Interplay of troponin- and myosin-based pathways of calcium activation in skeletal and cardiac muscle: the use of W7 as an inhibitor of thin filament activation. Biophys. J.86, 359–370 (2004). ArticleCASPubMedPubMed CentralGoogle Scholar
- Li, M. X., Hoffman, R. M. & Sykes, B. D. Interaction of cardiac troponin C with calmodulin antagonist [corrected] W7 in the presence of three functional regions of cardiac troponin I. Biochemistry45, 9833–9840 (2006). ArticleCASPubMedGoogle Scholar
- Oleszczuk, M., Robertson, I. M., Li, M. X. & Sykes, B. D. Solution structure of the regulatory domain of human cardiac troponin C in complex with the switch region of cardiac troponin I and W7: the basis of W7 as an inhibitor of cardiac muscle contraction. J. Mol. Cell Cardiol.48, 925–933 (2010). ArticleCASPubMedPubMed CentralGoogle Scholar
- Russell, A. J. et al. Activation of fast skeletal muscle troponin as a potential therapeutic approach for treating neuromuscular diseases. Nature Med.18, 452–455 (2012). A demonstration of the troponin-binding properties and muscle-activating effects of tirasemtiv, the first high-affinity fast skeletal muscle troponin activator to be tested in clinical trials.ArticleCASPubMedGoogle Scholar
- Bauer, T. A. et al. Effect of tirasemtiv, a selective activator of the fast skeletal muscle troponin complex, in patients with peripheral artery disease. Vasc. Med.19, 297–306 (2014). ArticleCASPubMedGoogle Scholar
- Shefner, J. M., Watson, M. L., Meng, L. & Wolff, A. A. A study to evaluate safety and tolerability of repeated doses of tirasemtiv in patients with amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Frontotemporal Degener.14, 574–581 (2013). ArticleCASPubMedGoogle Scholar
- de Winter, J. M. et al. Troponin activator augments muscle force in nemaline myopathy patients with nebulin mutations. J. Med. Genet.50, 383–392 (2013). ArticlePubMedGoogle Scholar
- Spyracopoulos, L. et al. Calcium-induced structural transition in the regulatory domain of human cardiac troponin C. Biochemistry36, 12138–12146 (1997). ArticleCASPubMedGoogle Scholar
- Herron, T. J. et al. Ca 2+ -independent positive molecular inotropy for failing rabbit and human cardiac muscle by α-myosin motor gene transfer. FASEB J.24, 415–424 (2010). ArticleCASPubMedPubMed CentralGoogle Scholar
- Day, S. M. et al. Histidine button engineered into cardiac troponin I protects the ischemic and failing heart. Nature Med.12, 181–189 (2006). ArticleCASPubMedGoogle Scholar
- Merkulov, S., Chen, X., Chandler, M. P. & Stelzer, J. E. In vivo cardiac myosin binding protein C gene transfer rescues myofilament contractile dysfunction in cardiac myosin binding protein C null mice. Circ. Heart Fail.5, 635–644 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Mearini, G. et al. Mybpc3 gene therapy for neonatal cardiomyopathy enables long-term disease prevention in mice. Nature Commun.5, 5515 (2014). ArticleCASGoogle Scholar
- Mamidi, R., Li, J., Gresham, K. S. & Stelzer, J. E. Cardiac myosin binding protein-C: a novel sarcomeric target for gene therapy. Pflugers Arch.466, 225–230 (2014). ArticleCASPubMedGoogle Scholar
- Maron, B. J., Maron, M. S. & Semsarian, C. Genetics of hypertrophic cardiomyopathy after 20 years: clinical perspectives. J. Am. Coll. Cardiol.60, 705–715 (2012). ArticlePubMedGoogle Scholar
- Sen-Chowdhry, S., Syrris, P. & McKenna, W. J. Genetics of restrictive cardiomyopathy. Heart Fail. Clin.6, 179–186 (2010). ArticlePubMedGoogle Scholar
- Sanbe, A. Dilated cardiomyopathy: a disease of the myocardium. Biol. Pharm. Bull.36, 18–22 (2013). ArticleCASPubMedGoogle Scholar
- McNally, E. M., Golbus, J. R. & Puckelwartz, M. J. Genetic mutations and mechanisms in dilated cardiomyopathy. J. Clin. Invest.123, 19–26 (2013). ArticleCASPubMedPubMed CentralGoogle Scholar
- Goldfarb, L. G. & Dalakas, M. C. Tragedy in a heartbeat: malfunctioning desmin causes skeletal and cardiac muscle disease. J. Clin. Invest.119, 1806–1813 (2009). ArticleCASPubMedPubMed CentralGoogle Scholar
- Teekakirikul, P., Kelly, M. A., Rehm, H. L., Lakdawala, N. K. & Funke, B. H. Inherited cardiomyopathies: molecular genetics and clinical genetic testing in the postgenomic era. J. Mol. Diagn.15, 158–170 (2013). ArticlePubMedGoogle Scholar
- Laing, N. G. & Nowak, K. J. When contractile proteins go bad: the sarcomere and skeletal muscle disease. Bioessays27, 809–822 (2005). ArticleCASPubMedGoogle Scholar
- Tajsharghi, H. & Oldfors, A. Myosinopathies: pathology and mechanisms. Acta Neuropathol.125, 3–18 (2013). ArticleCASPubMedGoogle Scholar
- Wallgren-Pettersson, C., Sewry, C. A., Nowak, K. J. & Laing, N. G. Nemaline myopathies. Semin. Pediatr. Neurol.18, 230–238 (2011). ArticlePubMedGoogle Scholar
- Lehtokari, V. L. et al. Identification of 45 novel mutations in the nebulin gene associated with autosomal recessive nemaline myopathy. Hum. Mutat.27, 946–956 (2006). ArticleCASPubMedGoogle Scholar
- Lawlor, M. W. et al. Novel mutations in NEB cause abnormal nebulin expression and markedly impaired muscle force generation in severe nemaline myopathy. Skelet. Muscle1, 23 (2011). ArticleCASPubMedPubMed CentralGoogle Scholar
- Claeys, K. G. & Fardeau, M. Myofibrillar myopathies. Handb. Clin. Neurol.113, 1337–1342 (2013). ArticlePubMedGoogle Scholar
- de Tombe, P. P. et al. Myofilament length dependent activation. J. Mol. Cell Cardiol.48, 851–858 (2010). ArticleCASPubMedPubMed CentralGoogle Scholar
- Kontrogianni-Konstantopoulos, A., Ackermann, M. A., Bowman, A. L., Yap, S. V. & Bloch, R. J. Muscle giants: molecular scaffolds in sarcomerogenesis. Physiol. Rev.89, 1217–1267 (2009). ArticleCASPubMedGoogle Scholar
- Mateja, R. D. & de Tombe, P. P. Myofilament length-dependent activation develops within 5 ms in guinea-pig myocardium. Biophys. J.103, L13–L15 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Zhang, Z. et al. Comparison of the Young–Laplace law and finite element based calculation of ventricular wall stress: implications for postinfarct and surgical ventricular remodeling. Ann. Thorac. Surg.91, 150–156 (2011). ArticlePubMedPubMed CentralGoogle Scholar
- Rudolf, R. et al. Alterations of cAMP-dependent signaling in dystrophic skeletal muscle. Front. Physiol.4, 290 (2013). ArticlePubMedPubMed CentralGoogle Scholar
- Lygren, B. & Tasken, K. Compartmentalized cAMP signalling is important in the regulation of Ca 2+ cycling in the heart. Biochem. Soc. Trans.34, 489–491 (2006). ArticleCASPubMedGoogle Scholar
- Boontje, N. M. et al. Enhanced myofilament responsiveness upon β-adrenergic stimulation in post-infarct remodeled myocardium. J. Mol. Cell Cardiol.50, 487–499 (2011). ArticleCASPubMedGoogle Scholar
- Gautel, M., Zuffardi, O., Freiburg, A. & Labeit, S. Phosphorylation switches specific for the cardiac isoform of myosin binding protein-C: a modulator of cardiac contraction? EMBO J.14, 1952–1960 (1995). ArticleCASPubMedPubMed CentralGoogle Scholar
- Gruen, M. Prinz, H. & Gautel, M. cAPK-phosphorylation controls the interaction of the regulatory domain of cardiac myosin binding protein C with myosin-S2 in an on-off fashion. FEBS Lett.453, 254–259 (1999). ArticleCASPubMedGoogle Scholar
- Kruger, M. & Linke, W. A. Protein kinase-A phosphorylates titin in human heart muscle and reduces myofibrillar passive tension. J. Muscle Res. Cell. Motil.27, 435–444 (2006). ArticleCASPubMedGoogle Scholar
- Solaro, R. J., Moir, A. J. & Perry, S. V. Phosphorylation of troponin I and the inotropic effect of adrenaline in the perfused rabbit heart. Nature262, 615–617 (1976). ArticleCASPubMedGoogle Scholar
- Wijnker, P. J. et al. Impact of site-specific phosphorylation of protein kinase A sites Ser23 and Ser24 of cardiac troponin I in human cardiomyocytes. Am. J. Physiol. Heart Circ. Physiol.304, H260–H268 (2013). ArticleCASPubMedGoogle Scholar
- Hamdani, N. et al. Distinct myocardial effects of beta-blocker therapy in heart failure with normal and reduced left ventricular ejection fraction. Eur. Heart J.30, 1863–1872 (2009). This article shows that increased calcium sensitivity is observed in heart tissue from both HFrEF and HFpEF patients. This is attributed to decreased phosphorylation of troponin I, which is further enhanced byβ1-adrenoceptor blockade.ArticleCASPubMedGoogle Scholar
- van Dijk, S. J. et al. A piece of the human heart: variance of protein phosphorylation in left ventricular samples from end-stage primary cardiomyopathy patients. J. Muscle Res. Cell. Motil.30, 299–302 (2009). ArticleCASPubMedGoogle Scholar
- MacIntosh, B. R., Holash, R. J. & Renaud, J. M. Skeletal muscle fatigue — regulation of excitation-contraction coupling to avoid metabolic catastrophe. J. Cell Sci.125, 2105–2114 (2012). CASPubMedGoogle Scholar
- Kamm, K. E. & Stull, J. T. Signaling to myosin regulatory light chain in sarcomeres. J. Biol. Chem.286, 9941–9947 (2011). ArticleCASPubMedPubMed CentralGoogle Scholar
- Scruggs, S. B. & Solaro, R. J. The significance of regulatory light chain phosphorylation in cardiac physiology. Arch. Biochem. Biophys.510, 129–134 (2011). ArticleCASPubMedPubMed CentralGoogle Scholar
- Grimm, M. et al. Key role of myosin light chain (MLC) kinase-mediated MLC2a phosphorylation in the α1-adrenergic positive inotropic effect in human atrium. Cardiovasc. Res.65, 211–220 (2005). ArticleCASPubMedGoogle Scholar
- Flashman, E., Redwood, C., Moolman-Smook, J. & Watkins, H. Cardiac myosin binding protein C: its role in physiology and disease. Circ. Res.94, 1279–1289 (2004). ArticleCASPubMedGoogle Scholar
- Lowey, S., Slayter, H. S., Weeds, A. G. & Baker, H. Substructure of the myosin molecule. I. Subfragments of myosin by enzymic degradation. J. Mol. Biol.42, 1–29 (1969). ArticleCASPubMedGoogle Scholar
- Al-Khayat, H. A., Kensler, R. W., Squire, J. M., Marston, S. B. & Morris, E. P. Atomic model of the human cardiac muscle myosin filament. Proc. Natl Acad. Sci. USA110, 318–323 (2013). ArticleCASPubMedGoogle Scholar
- Craig, R. & Woodhead, J. L. Structure and function of myosin filaments. Curr. Opin. Struct. Biol.16, 204–212 (2006). ArticleCASPubMedGoogle Scholar
- Weeds, A. G. & Lowey, S. Substructure of the myosin molecule. II. The light chains of myosin. J. Mol. Biol.61, 701–725 (1971). ArticleCASPubMedGoogle Scholar
- Freiburg, A. & Gautel, M. A molecular map of the interactions between titin and myosin-binding protein C. Implications for sarcomeric assembly in familial hypertrophic cardiomyopathy. Eur. J. Biochem.235, 317–323 (1996). ArticleCASPubMedGoogle Scholar
- Miyamoto, C. A., Fischman, D. A. & Reinach, F. C. The interface between MyBP-C and myosin: site-directed mutagenesis of the CX myosin-binding domain of MyBP-C. J. Muscle Res. Cell. Motil.20, 703–715 (1999). ArticleCASPubMedGoogle Scholar
- Bhuiyan, M. S., Gulick, J., Osinska, H., Gupta, M. & Robbins, J. Determination of the critical residues responsible for cardiac myosin binding protein C's interactions. J. Mol. Cell Cardiol.53, 838–847 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Sousa, D. R., Stagg, S. M. & Stroupe, M. E. Cryo-EM structures of the actin:tropomyosin filament reveal the mechanism for the transition from C- to M-state. J. Mol. Biol.425, 4544–4555 (2013). ArticleCASPubMedGoogle Scholar
- White, S. P., Cohen, C. & Phillips, G. N. J. Structure of co-crystals of tropomyosin and troponin. Nature325, 826–828 (1987). ArticleCASPubMedGoogle Scholar
- Gourinath, S. et al. Crystal structure of scallop myosin s1 in the pre-power stroke state to 2.6 Å resolution: flexibility and function in the head. Structure11, 1621–1627 (2003). ArticleCASPubMedGoogle Scholar
- Behrmann, E. et al. Structure of the rigor actin–tropomyosin–myosin complex. Cell150, 327–338 (2012). An 8 Å-resolution description of the actin–tropomyosin–myosin complex by cryo-electron microscopy, identifying key residues implicated in myopathies. The authors present a detailed model of how actin binding to myosin induces phosphate and nucleotide release and initiation of the power stroke.ArticleCASPubMedPubMed CentralGoogle Scholar
- Sia, S. K. et al. Structure of cardiac muscle troponin C unexpectedly reveals a closed regulatory domain. J. Biol. Chem.272, 18216–18221 (1997). ArticleCASPubMedGoogle Scholar
- Eichmuller, C. & Skrynnikov, N. R. A new amide proton R1ρ experiment permits accurate characterization of microsecond time-scale conformational exchange. J. Biomol. NMR32, 281–293 (2005). ArticleCASPubMedGoogle Scholar
- Geisterfer-Lowrance, A. A. et al. A molecular basis for familial hypertrophic cardiomyopathy: a β cardiac myosin heavy chain gene missense mutation. Cell62, 999–1006 (1990). ArticleCASPubMedGoogle Scholar
- Hernandez, O. M., Jones, M., Guzman, G. & Szczesna-Cordary, D. Myosin essential light chain in health and disease. Am. J. Physiol. Heart Circ. Physiol.292, H1643–H1654 (2007). ArticleCASPubMedGoogle Scholar
- Poetter, K. et al. Mutations in either the essential or regulatory light chains of myosin are associated with a rare myopathy in human heart and skeletal muscle. Nature Genet.13, 63–69 (1996). ArticleCASPubMedGoogle Scholar
- Ha, K. et al. MYBPC1 mutations impair skeletal muscle function in zebrafish models of arthrogryposis. Hum. Mol. Genet.22, 4967–4977 (2013). ArticleCASPubMedPubMed CentralGoogle Scholar
- Schlossarek, S., Mearini, G. & Carrier, L. Cardiac myosin-binding protein C in hypertrophic cardiomyopathy: mechanisms and therapeutic opportunities. J. Mol. Cell Cardiol.50, 613–620 (2011). ArticleCASPubMedGoogle Scholar
- Marston, S., Copeland, O., Gehmlich, K., Schlossarek, S. & Carrier, L. How do MYBPC3 mutations cause hypertrophic cardiomyopathy? J. Muscle Res. Cell. Motil.33, 75–80 (2012). ArticleCASPubMedGoogle Scholar
- Watkins, H. et al. Mutations in the cardiac myosin binding protein-C gene on chromosome 11 cause familial hypertrophic cardiomyopathy. Nature Genet.11, 434–437 (1995). ArticleCASPubMedGoogle Scholar
- Herman, D. S. et al. Truncations of titin causing dilated cardiomyopathy. N. Engl. J. Med.366, 619–628 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Chauveau, C. et al. Recessive TTN truncating mutations define novel forms of core myopathy with heart disease. Hum. Mol. Genet.23, 980–991 (2013). ArticlePubMedPubMed CentralCASGoogle Scholar
- Wang, K., McClure, J. & Tu, A. Titin: major myofibrillar components of striated muscle. Proc. Natl Acad. Sci. USA76, 3698–3702 (1979). ArticleCASPubMedPubMed CentralGoogle Scholar
- Nowak, K. J. et al. Mutations in the skeletal muscle α-actin gene in patients with actin myopathy and nemaline myopathy. Nature Genet.23, 208–212 (1999). ArticleCASPubMedGoogle Scholar
- Mogensen, J. et al. Clinical and genetic characteristics of α cardiac actin gene mutations in hypertrophic cardiomyopathy. J. Med. Genet.41, e10 (2004). ArticleCASPubMedPubMed CentralGoogle Scholar
- Watkins, H. et al. Mutations in the genes for cardiac troponin T and α-tropomyosin in hypertrophic cardiomyopathy. N. Engl. J. Med.332, 1058–1064 (1995). ArticleCASPubMedGoogle Scholar
- Donner, K. et al. Mutations in the β-tropomyosin (TPM2) gene—a rare cause of nemaline myopathy. Neuromuscul. Disord.12, 151–158 (2002). ArticlePubMedGoogle Scholar
- Sung, S. S. et al. Mutations in genes encoding fast-twitch contractile proteins cause distal arthrogryposis syndromes. Am. J. Hum. Genet.72, 681–690 (2003). ArticleCASPubMedPubMed CentralGoogle Scholar
- Kee, A. J. & Hardeman, E. C. Tropomyosins in skeletal muscle diseases. Adv. Exp. Med. Biol.644, 143–157 (2008). ArticleCASPubMedGoogle Scholar
- Laing, N. G. et al. A mutation in the α tropomyosin gene TPM3 associated with autosomal dominant nemaline myopathy. Nature Genet.9, 75–79 (1995). ArticleCASPubMedGoogle Scholar
- Johnston, J. J. et al. A novel nemaline myopathy in the Amish caused by a mutation in troponin T1. Am. J. Hum. Genet.67, 814–821 (2000). ArticleCASPubMedPubMed CentralGoogle Scholar
- Sung, S. S. et al. Mutations in TNNT3 cause multiple congenital contractures: a second locus for distal arthrogryposis type 2B. Am. J. Hum. Genet.73, 212–214 (2003). ArticlePubMedPubMed CentralGoogle Scholar
- Kimura, A. et al. Mutations in the cardiac troponin I gene associated with hypertrophic cardiomyopathy. Nature Genet.16, 379–382 (1997). ArticleCASPubMedGoogle Scholar
- Landstrom, A. P. et al. Molecular and functional characterization of novel hypertrophic cardiomyopathy susceptibility mutations in TNNC1-encoded troponin C. J. Mol. Cell Cardiol45, 281–288 (2008). ArticleCASPubMedPubMed CentralGoogle Scholar
- Purevjav, E. et al. Nebulette mutations are associated with dilated cardiomyopathy and endocardial fibroelastosis. J. Am. Coll. Cardiol56, 1493–1502 (2010). ArticlePubMedPubMed CentralGoogle Scholar
- Pappas, C. T., Bliss, K. T., Zieseniss, A. & Gregorio, C. C. The nebulin family: an actin support group. Trends Cell Biol.21, 29–37 (2011). ArticleCASPubMedGoogle Scholar
- Millevoi, S. et al. Characterization of nebulette and nebulin and emerging concepts of their roles for vertebrate Z-discs. J. Mol. Biol.282, 111–123 (1998). ArticleCASPubMedGoogle Scholar
- Luther, P. K. The vertebrate muscle Z-disc: sarcomere anchor for structure and signalling. J. Muscle Res. Cell. Motil.30, 171–185 (2009). ArticlePubMedPubMed CentralGoogle Scholar
- Chiu, C. et al. Mutations in α-actinin-2 cause hypertrophic cardiomyopathy: a genome-wide analysis. J. Am. Coll. Cardiol.55, 1127–1135 (2010). ArticleCASPubMedGoogle Scholar
- Moreira, E. S. et al. Limb-girdle muscular dystrophy type 2G is caused by mutations in the gene encoding the sarcomeric protein telethonin. Nature Genet.24, 163–166 (2000). ArticleCASPubMedGoogle Scholar
- Hayashi, T. et al. Tcap gene mutations in hypertrophic cardiomyopathy and dilated cardiomyopathy. J. Am. Coll. Cardiol.44, 2192–2201 (2004). ArticleCASPubMedGoogle Scholar
- Razinia, Z., Makela, T., Ylanne, J. & Calderwood, D. A. Filamins in mechanosensing and signaling. Annu. Rev. Biophys.41, 227–246 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Vorgerd, M. et al. A mutation in the dimerization domain of filamin c causes a novel type of autosomal dominant myofibrillar myopathy. Am. J. Hum. Genet.77, 297–304 (2005). ArticleCASPubMedPubMed CentralGoogle Scholar
- Faulkner, G. et al. FATZ, a filamin-, actinin-, and telethonin-binding protein of the Z-disc of skeletal muscle. J. Biol. Chem.275, 41234–41242 (2000). ArticleCASPubMedGoogle Scholar
- Osio, A. et al. Myozenin 2 is a novel gene for human hypertrophic cardiomyopathy. Circ. Res.100, 766–768 (2007). ArticleCASPubMedPubMed CentralGoogle Scholar
- Purevjav, E. et al. Molecular basis for clinical heterogeneity in inherited cardiomyopathies due to myopalladin mutations. Hum. Mol. Genet.21, 2039–2053 (2012). ArticleCASPubMedPubMed CentralGoogle Scholar
- Meyer, T. et al. Novel mutations in the sarcomeric protein myopalladin in patients with dilated cardiomyopathy. Eur. J. Hum. Genet.21, 294–300 (2013). ArticleCASPubMedGoogle Scholar
- Bang, M. L. et al. Myopalladin, a novel 145-kilodalton sarcomeric protein with multiple roles in Z-disc and I-band protein assemblies. J. Cell Biol.153, 413–427 (2001). ArticleCASPubMedPubMed CentralGoogle Scholar
- Salmikangas, P. et al. Myotilin, the limb-girdle muscular dystrophy 1A (LGMD1A) protein, cross-links actin filaments and controls sarcomere assembly. Hum. Mol. Genet.12, 189–203 (2003). ArticleCASPubMedGoogle Scholar
- Hauser, M. A. et al. Myotilin is mutated in limb girdle muscular dystrophy 1A. Hum. Mol. Genet.9, 2141–2147 (2000). ArticleCASPubMedGoogle Scholar
- Selcen, D. & Engel, A. G. Mutations in myotilin cause myofibrillar myopathy. Neurology62, 1363–1371 (2004). ArticleCASPubMedGoogle Scholar
- von Nandelstadh, P. et al. A class III PDZ binding motif in the myotilin and FATZ families binds enigma family proteins: a common link for Z-disc myopathies. Mol. Cell. Biol.29, 822–834 (2009). ArticleCASPubMedGoogle Scholar
- Strach, K. et al. ZASPopathy with childhood-onset distal myopathy. J. Neurol.259, 1494–1496 (2012). ArticlePubMedGoogle Scholar
- Selcen, D. & Engel, A. G. Mutations in ZASP define a novel form of muscular dystrophy in humans. Ann. Neurol.57, 269–276 (2005). ArticleCASPubMedGoogle Scholar
- Vatta, M. et al. Mutations in Cypher/ZASP in patients with dilated cardiomyopathy and left ventricular non-compaction. J. Am. Coll. Cardiol.42, 2014–2027 (2003). ArticleCASPubMedGoogle Scholar
- Arimura, T. et al. A Cypher/ZASP mutation associated with dilated cardiomyopathy alters the binding affinity to protein kinase C. J. Biol. Chem.279, 6746–6752 (2004). ArticleCASPubMedGoogle Scholar
- Lin, C. et al. Cypher/ZASP is a novel A-kinase anchoring protein. J. Biol. Chem.288, 29403–29413 (2013). ArticleCASPubMedPubMed CentralGoogle Scholar
- Limouze, J., Straight, A. F., Mitchison, T. & Sellers, J. R. Specificity of blebbistatin, an inhibitor of myosin II. J. Muscle Res. Cell. Motil.25, 337–341 (2004). ArticleCASPubMedGoogle Scholar
- Cheung, A. et al. A small-molecule inhibitor of skeletal muscle myosin II. Nature Cell Biol.4, 83–88 (2002). ArticleCASPubMedGoogle Scholar
- McKillop, D. F., Fortune, N. S., Ranatunga, K. W. & Geeves, M. A. The influence of 2,3-butanedione 2-monoxime (BDM) on the interaction between actin and myosin in solution and in skinned muscle fibres. J. Muscle Res. Cell. Motil.15, 309–318 (1994). ArticleCASPubMedGoogle Scholar
- Kischel, P., Stevens, L. & Mounier, Y. Differential effects of bepridil on functional properties of troponin C in slow and fast skeletal muscles. Br. J. Pharmacol.128, 767–773 (1999). ArticleCASPubMedPubMed CentralGoogle Scholar
- Robertson, I. M., Sun, Y. B., Li, M. X. & Sykes, B. D. A structural and functional perspective into the mechanism of Ca 2+ -sensitizers that target the cardiac troponin complex. J. Mol. Cell Cardiol.49, 1031–1041 (2010). ArticleCASPubMedPubMed CentralGoogle Scholar
Acknowledgements
The authors' work is supported by Heart and Stroke Foundation of Canada, grant-in-aid G-14-0005884, and the Canadian Institutes of Health Research, operating grant 37769.